Multiple Sclerosis (MS) - Multiple Sclerosis Causes & Treatment
Multiple sclerosis (abbreviated MS, also known as disseminated sclerosis or encephalomyelitis disseminata) is an autoimmune condition in which the immune system attacks the central nervous system, leading to demyelination. Disease onset usually occurs in young adults, and it is more common in females. It has a prevalence that ranges between 2 and 150 per 100,000
What is Multiple sclerosis?
Multiple sclerosis (MS) is a nervous system disease that affects your brain and spinal cord. It damages the myelin sheath, the material that surrounds and protects your nerve cells. This damage slows down or block messages between your brain and your body, leading to the symptoms of Multiple sclerosis (MS). They can include
-
Visual disturbances
-
Muscle weakness
-
Trouble with coordination and balance
-
Sensations such as numbness, prickling, or "pins and needles"
-
Thinking and memory problems
Causes of Multiple Sclerosis
No one knows what causes Multiple sclerosis (MS). It may be an autoimmune disease, which happens when your body attacks itself. Multiple sclerosis affects women more than men. It often begins between the ages of 20 and 40. Usually, the disease is mild, but some people lose the ability to write, speak or walk. There is no cure for multiple sclerosis (MS), but medicines may slow it down and help control symptoms. Physical and occupational therapy may also help.
-
Multiple Sclerosis is not considered a hereditary disease. However, a number of genetic variations have been shown to increase the risk of developing the disease. The risk of acquiring Multiple Sclerosis (MS) is higher in relatives of a person with the disease than in the general population, especially in the case of siblings, parents, and children.
-
Multiple Sclerosis is more common in people who live farther from the equator. Decreased sunlight exposure has been linked with a higher risk of Multiple Sclerosis. Decreased vitamin D production and intake has been the main biological mechanism used to explain the higher risk among those less exposed to sun.
-
Severe stress may also be a risk factor although evidence is weak; parents who lost a child unexpectedly were more likely to develop MS (multiple sclerosis) than parents who had not.
-
Smoking has also been shown to be an independent risk factor for developing Multiple sclerosis (MS).
Multiple Sclerosis was first described in 1868 by Jean-Martin Charcot. Multiple Sclerosis (MS) affects the ability of nerve cells in the brain and spinal cord to communicate with each other. Nerve cells communicate by sending electrical signals called action potentials down long fibers called axons, which are wrapped in an insulating substance called myelin. In MS, the body's own immune system attacks and damages the myelin. When myelin is lost, the axons can no longer effectively conduct signals. The name multiple sclerosis refers to scars ( scleroses – better known as plaques or lesions) in the white matter of the brain and spinal cord, which is mainly composed of myelin. Although much is known about the mechanisms involved in the disease process, the cause remains unknown. Theories include genetics or infections. Different environmental risk factors have also been found.
Symptoms of Multiple Sclerosis
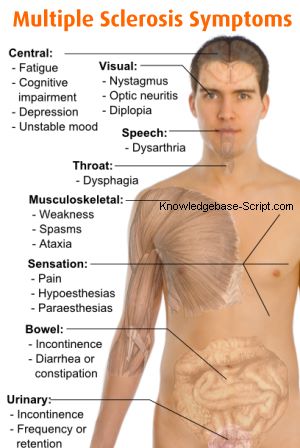 Almost any neurological symptom can appear with the disease, and often progresses to physical and cognitive disability. Symptoms of Multiple Sclerosis (MS) usually appear in episodic acute periods of worsening (relapses, exacerbations, bouts or attacks), in a gradually-progressive deterioration of neurologic function, or in a combination of both. Multiple Sclerosis takes several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or slowly accumulating over time (progressive forms). Between attacks, symptoms may go away completely, but permanent neurological problems often occur, especially as the disease advances.
Almost any neurological symptom can appear with the disease, and often progresses to physical and cognitive disability. Symptoms of Multiple Sclerosis (MS) usually appear in episodic acute periods of worsening (relapses, exacerbations, bouts or attacks), in a gradually-progressive deterioration of neurologic function, or in a combination of both. Multiple Sclerosis takes several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or slowly accumulating over time (progressive forms). Between attacks, symptoms may go away completely, but permanent neurological problems often occur, especially as the disease advances.
The most common presentation of MS (Multiple Sclerosis) is the clinically isolated syndrome (CIS). In CIS, a patient has an attack suggestive of demyelination, but does not fulfill the criteria for multiple sclerosis. Only 30 to 70% of persons experiencing CIS later develop MS. The disease usually presents with sensorial (46% of cases), visual (33%), cerebellar (30%) and motor (26%) symptoms. Many rare initial symptoms have also been reported, including aphasia, psychosis, and epilepsy. Patients first seeking medical attention commonly present with multiple symptoms. The initial signs and symptoms of MS are often transient, mild, and self-limited. These signs and symptoms often do not prompt a person to seek medical attention and are sometimes identified only retrospectively once the diagnosis of MS has been made. Cases of MS are sometimes incidentally identified during neurological examinations performed for other causes. Such cases are referred to as subclinical MS.
Nystagmus, characterised by involuntary eye movements, is one of many symptoms that can appear with Multiple Sclerosis (MS). The person with MS can suffer almost any neurological symptom or sign, including changes in sensation (hypoesthesia and paraesthesia), muscle weakness, muscle spasms, or difficulty in moving; difficulties with coordination and balance (ataxia); problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis, or diplopia), fatigue, acute or chronic pain, and bladder and bowel difficulties. Cognitive impairment of varying degrees and emotional symptoms of depression or unstable mood are also common. The main clinical measure of disability progression and symptom severity is the Expanded Disability Status Scale or EDSS.
Multiple sclerosis relapses are often unpredictable, occurring without warning and without obvious inciting factors. Some attacks, however, are preceded by common triggers. Relapses occur more frequently during spring and summer. Infections such as the common cold, influenza, or gastroenteritis increase the risk of relapse. Stress may also trigger an attack. Pregnancy may affect susceptibility to relapse, offering protection during the last trimester, for instance. During the first few months after delivery, however, the risk of relapse is increased. Overall, pregnancy does not seem to influence long-term disability. Many potential triggers have been examined and found not to influence MS relapse rates. There is no evidence that vaccination for influenza, hepatitis B, varicella, tetanus, or tuberculosis increases the risk of relapse. Physical trauma does not trigger relapses. Exposure to higher than usual ambient temperatures can exacerbate extant symptoms, an effect known as Uhthoff's phenomenon. Uhthoff's phenomenon is not, however, an established relapse trigger.
Multiple Sclerosis Treatment
There is no known cure for Multiple Sclerosis (MS). Treatments attempt to return function after an attack, prevent new attacks, and prevent disability. Multiple Sclerosis medications can have adverse effects or be poorly tolerated, and many patients pursue alternative treatments, despite the lack of supporting scientific study. The prognosis is difficult to predict; it depends on the subtype of the disease, the individual patient's disease characteristics, the initial symptoms and the degree of disability the person experiences as time advances. Life expectancy of patients is nearly the same as that of the unaffected population.
Alternative Treatments for Multiple Sclerosis
As with most chronic diseases, alternative treatments are pursued by some patients, despite the shortage of supporting, comparable, replicated scientific study. Examples are dietary regimens, herbal medicine, including the use of medical cannabis to help alleviate symptoms, and hyperbaric oxygenation. The therapeutic practice of martial arts such as tai chi, relaxation disciplines such as yoga, or general exercise seems to mitigate fatigue but has no effect on cognitive function.